What is Candida Auris? A fancy type of foreign dance? A natural light display in the northern sky presenting beautiful colors at certain times of the year? An emerging fungus presenting a serious global health threat?
In March of this year, the US Centers for Disease Control and Prevention (CDC) issued a warning on Candida Auris (C. auris) due to spreading at an alarming rate throughout U.S. health-care facilities, C. auris is considered an “urgent antimicrobial resistance threat.” The CDC threat level of “urgent” is the highest level, requiring quick and aggressive action. Other, more familiar organisms listed in the “urgent” category are Clostridioides difficile (C. diff), Carbapenem-resistant Acinetobacter baumannii (CRAB), Neisseria gonorrhoeae and Carbapenem-resistant Enterobacteriaceae (CRE).
What makes C. auris so concerning?
- Rapid spread.
- Surface survival time.
- Resistance.
- High mortality.
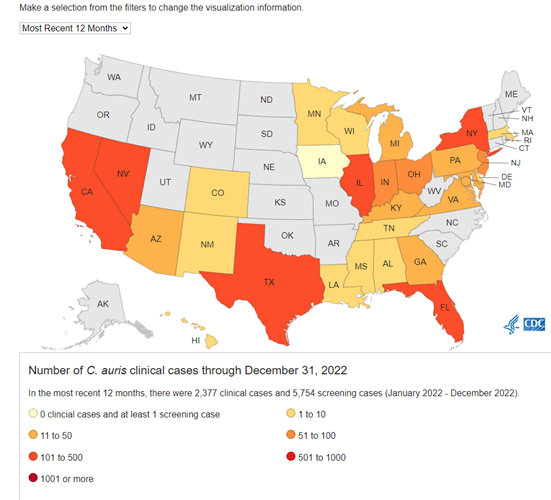
Information continues to be discovered, but according to literature, Candida Auris was first isolated from the external ear canal of a hospitalized patient in Tokyo, Japan in 2009. Candida meaning “parasitic fungi that resembles yeast” and auris which is Latin for “ear.” As past data was reviewed, it was found that the earliest known strains dated back to 1996 in South Korea. According to an article published in The Lancet in May 2023, C. auris has spread to over thirty countries and all continents except Antarctica. The following graphic was taken from the CDC’s Tracking C. auris interactive map found here. It shows spread of C. auris in the United States over the previous 12 months.
C. auris tends to spread rapidly in healthcare environments, particularly in high acuity care facilities such as hospitals, long-term acute care facilities and ventilator capable nursing homes. It spreads both directly and indirectly through contact with surfaces in the patient care environment and has been shown to live on glass surfaces for around 3 days, steel surfaces for greater than 7 days and plastic surfaces for greater than 14 days. Length of stay has been shown to increase transmission risk, but transmission has occurred in as little as 4 hours. According to an article in the New York Times from April 2019, the Brooklyn branch of Mount Sinai Hospital in New York City found C. auris contamination to be so extensive in a former patient’s room, Dr. Scott Lorin, the hospital’s president stated, “they needed special cleaning equipment and had to remove ceiling and floor tiles to eradicate it. Everything was positive—the walls, the bed, the doors, the curtains, the phones, the sink, the whiteboard, the poles, the pump.” According to Dr. Scott, also testing positive was the mattress, the bed rails, the canister holds, the window shades, the ceiling, everything in the room was positive.
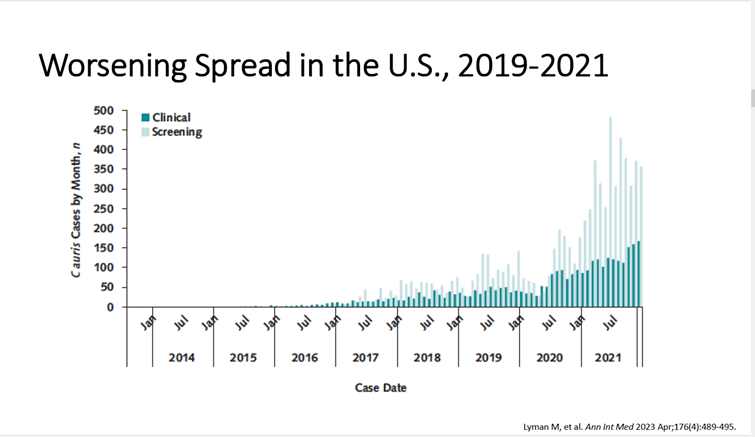
Because the skin promotes high biofilm formation, it facilitates spread. Patients with invasive devices, recent surgery, diabetes, recent broad-spectrum antibiotic or antifungal use are most affected by C. auris. C. auris has caused bloodstream, wound and ear infections and has also been isolated from respiratory and urine specimens but it’s unclear whether it causes infection in the lungs or bladder. It is easily spread also due to colonization, where patients have C. auris but show no signs and symptoms of infection and are not aware of it. Dr. Jennifer Hsu, an Infectious Disease Specialist granted permission for the use of the following graphic showing C. auris worsening spread in the United States from 2019-2021, displayed through clinical and screening cases.
Generally, C. auris is not a threat to healthy people, but can cause high mortality rates, especially in patients with a presence of other comorbidities and chronic health conditions. One of the reasons is due to its level of drug resistance. An overall crude mortality rate of around 34% has been estimated by the University of Minnesota’s Center for Infectious Disease Research and Policy (CIDRAP) Research and Innovation Office.
Currently there are three known classes of antifungals used to treat C. auris, and some isolates have been shown to be resistant to all 3 classes. Morbidity and Mortality Weekly Report: Transmission of Pan-Resistant and Echinocandin Resistant Candida auris in Health Care Facilities—Texas and the District of Columbia, January-April 2021, noted the following information:
- Azoles: 85% of C. auris isolates are resistant
- Polyenes: 33% of C. auris isolates are resistant
- Echinocandins: 1% of C. auris isolates are resistant
This article also stated, “Echinocandins are critical for treatment of C. auris infections and are recommended as first-line therapy for most invasive Candida infections.” Due to the concern of echinocandin resistance, however, the CDC does not recommend treatment of C. auris identified from non-invasive sites (colonized patients) when there is no active infection and is generally only clinically indicated when clinical disease is present.
What can we do?
According to the SD Department of Health on November 27, 2023, South Dakota has not seen any reported cases of C. auris. This is great news. Case numbers throughout the state continue to be monitored, however, due to the presence of C. auris in neighboring states. Awareness and alertness to its presence are key. According to the CDC, “In non-endemic settings, MDRO prevalence is expected to continue to rise despite the use of prevention strategies, but at a slower rate compared to if these strategies are not implemented.” You can find more about the CDC’s Containment Strategy here.
While information surrounding C. auris continues to develop, primary prevention methods revolve around basic infection control practices. These include:
- Diligent hand hygiene
- Thorough cleaning and disinfection of patient environment and equipment
- Implementing and maintaining transmission-based contact precautions when appropriate
- Meticulous skin prep prior to surgery
- Robust antimicrobial stewardship programs
- Caring for patient medical devices while following CDC guidelines
- Communicating C. auris status upon patient transfer
- Screening high risk patients (especially those with an overnight international healthcare stay, or overnight healthcare in a US area with high rates of C. auris—CA, NV, TX, FL, NY, Chicago area, Washington D.C. area)
- Screening of contacts of newly identified C. auris patients
- Lab surveillance
Due to the ability of C. auris to persist on multiple surfaces for extended periods of time, selection and use of disinfectants is very important. According to the CDC, quaternary ammonium products are not effective against C. auris. The CDC recommends use of a disinfectant specifically indicated to kill C. auris, or those on EPA’s ‘List P.’ Products on EPA’s ‘List K,’ are also acceptable if the products on ‘List P’ are unsuitable or unavailable.
Candida auris is an urgent health threat that is proving to be challenging to combat. With awareness, alertness and diligence, South Dakota’s medical facilities will be prepared when C. auris arrives. To find out more, please see the list of resources used in the compilation of this article.
Resources:
- Candida auris https://www.cdc.gov/fungal/candida-auris/index.html
- State of Iowa Department of Health and Human Services Webinar: Curb the Spread: Candida auris https://www.youtube.com/watch?v=1KP34HtAMwI
- Morbidity and Mortality Weekly Report July 23, 2021 Notes from the Field: Transmission of Pan-Resistant and Echinocandin-Resistant Candida auris in Health Care Facilities ― Texas and the District of Columbia, January–April 2021 https://www.cdc.gov/mmwr/volumes/70/wr/mm7029a2.htm
- Infection and Control for Candida auris https://www.cdc.gov/fungal/candida-auris/c-auris-infection-control.html
- Candida auris: An emerging fungus that presents a serious global health threat https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9986882/
- Emergence of resistant Candida auris https://www.thelancet.com/journals/lanmic/article/PIIS2666-5247(23)00143-X/fulltext
- A Mysterious Infection, Spanning the Globe in a Climate of Secrecy https://www.nytimes.com/2019/04/06/health/drug-resistant-candida-auris.html
- Annals of Internal Medicine Worsening Spread of Candida auris in the United States, 2019-2021 https://pubmed.ncbi.nlm.nih.gov/36940442/
- Interim Guidance for Public Health Strategies to Prevent the Spread of Novel or Targeted Multidrug-resistant Organisms (MDROs) https://www.cdc.gov/hai/mdro-guides/prevention-strategy.html
- US hospital data show high death rate with Candida auris infections https://www.cidrap.umn.edu/antimicrobial-stewardship/us-hospital-data-show-high-death-rate-candida-auris-infections